Mental Illness and Drug Use: An Unfortunate Correlation
Substance abuse and mental health issues can both have a significant impact on an individual’s quality of life, and these struggles affect a surprising number of Americans. In 2014, over 44 million people reported using illicit drugs in the past year, and more than 60 million said they had engaged in binge drinking in the past month. Meanwhile, nearly 10 million reported experiencing a mental illness that led to serious functional impairment.
While both of these issues present serious public health concerns, they aren’t happening in isolation – drug addiction and mental health can be closely related issues. For many individuals, substance dependency and psychiatric disorders are co-occurring conditions, commonly known as a “dual diagnosis.” Drug and alcohol abuse can lead to the development of mental health conditions, and, at the same time, those experiencing psychiatric disorders may turn to substance use as a form of self-medication for their symptoms. Unfortunately, this means they now face two threats to their health and well-being – threats that may ultimately prove fatal.
So how common is this dual diagnosis? We’ve analyzed data from the WONDER dataset provided by the Centers for Disease Control, as well as population studies from the Substance Abuse and Mental Health Services Administration, to find trends in how substance use and mental health conditions are related. Read on to learn about the impact of these conditions across society.
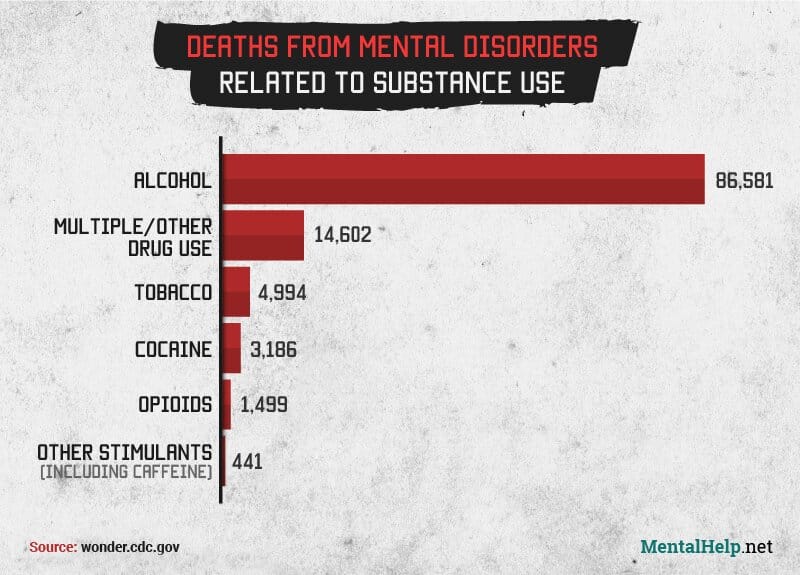
From 1999 to 2013, over 100,000 deaths were attributed to mental health disorders that were related to drug or alcohol use. By far the most common was alcohol: 86,581 deaths in total were linked to mental conditions that stemmed from drinking. Not only is binge drinking more common among Americans than illicit drug use, but it can also worsen the symptoms of depression and anxiety.
After alcohol, multiple or other drug use is associated with over 14,000 deaths from mental health disorders. This can include mental illnesses linked to an unspecified substance or several substances. Those who abuse multiple drugs concurrently can be at increased danger due to the unpredictable combined effects of these substances, and polydrug use is associated with a greater risk of anxiety disorder and suicide attempts.
Assessing for the directionality between substance abuse and other mental and behavioral health issues can be quite complicated. In some cases, people may be able to provide a medical history that reveals, with some certainty, that a mental health issue existed prior to substance use. Others who have been using drugs or abusing alcohol for a long while may more clearly recollect a later development of mental health symptoms such as depressed mood, or anxiety. Ultimately, making such a distinction may be more of an academic exercise than a practical one – treatment can commence even if the interplay is somewhat unclear. Dual diagnosis treatment techniques are evolving to benefit anyone struggling with both issues. Don’t let a potential dual diagnosis dissuade you from seeking addiction treatment. Resolve to finally seek treatment this year.
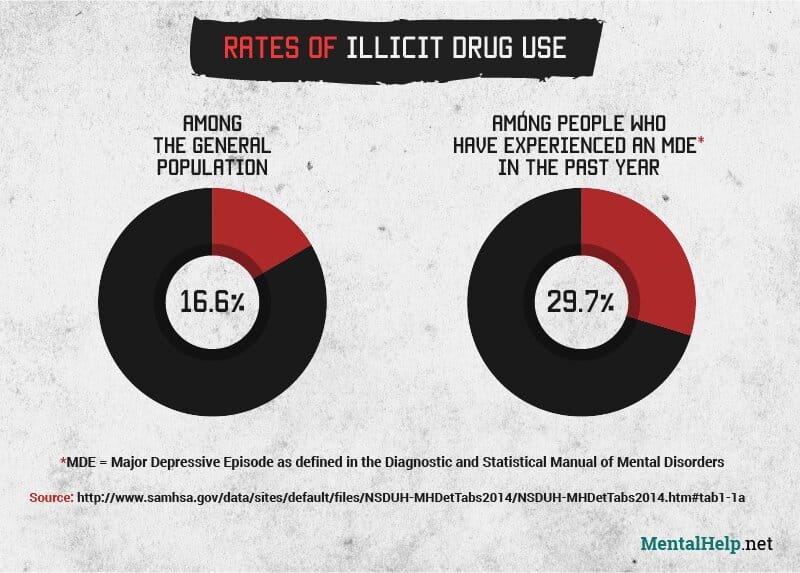
So what does the interaction of mental health and drug abuse look like? One way to study this is to compare drug use among the population overall and among those experiencing mental illnesses. The results are striking: While 16.6% of the population reported illicit drug use over the past year – a very high proportion already – this rises to 29.7% among those who experienced a major depressive episode during that time.
These episodes are defined by the Diagnostic and Statistical Manual of Mental Disorders as lasting at least two weeks, during which an individual experiences a lack of pleasure, depressed mood, and depressive symptoms. Just those criteria were enough to nearly double a person’s risk of engaging in drug use.
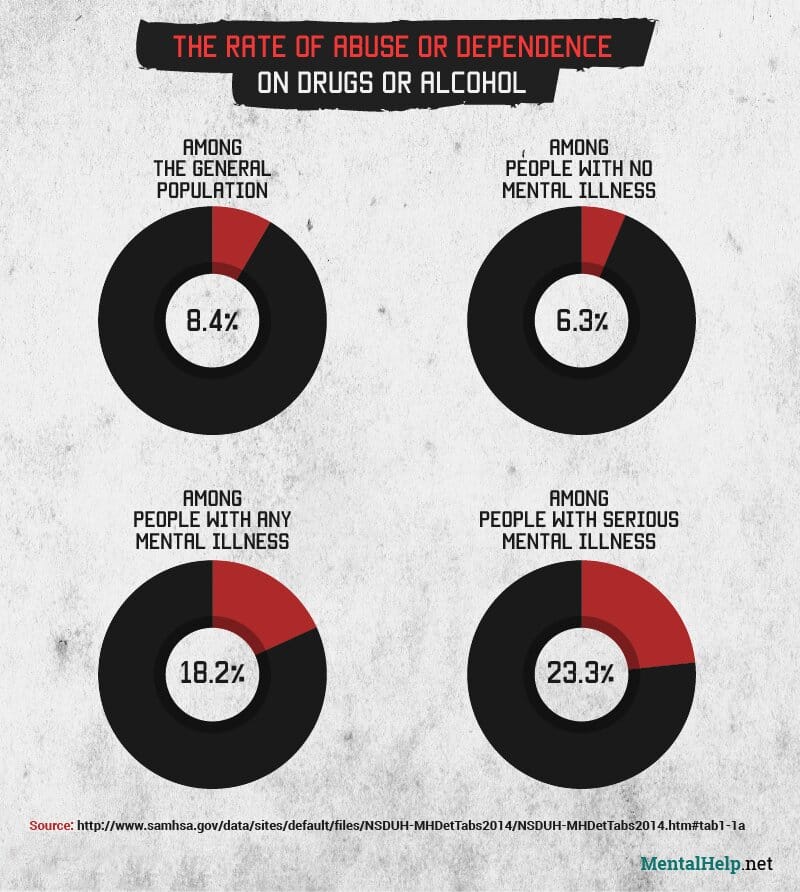
When we analyze the varying rates of substance abuse or dependence among those who’ve experienced no mental illness, any mental illness, or a serious mental illness, the trend is undeniable. Compared with the general population in 2014, people who hadn’t experienced a mental illness had only around three-quarters the rate of drug or alcohol abuse or dependence.
However, while only 6.3% of people with no mental illness reported abuse or dependence, this nearly tripled to 18.2% among those with any mental illness. And those who experienced a serious mental illness – defined as substantially interfering with a major life activity – showed almost quadruple the rate, at 23.3%.
On its own, the presence of a mental health condition or a drug and alcohol problem can have lasting, negative impacts to health and wellbeing. Dealing with both simultaneously – as is the case in a dual diagnosis situation – can be exceedingly tough for any individual to bear, as each condition may perpetuate, or worsen the issues brought by the other. These days, more and more programs are available to provide help for these situations. Treatment efforts, specifically tailored to an individual’s unique needs, can help to manage the struggle, and lay the groundwork for lasting recovery.
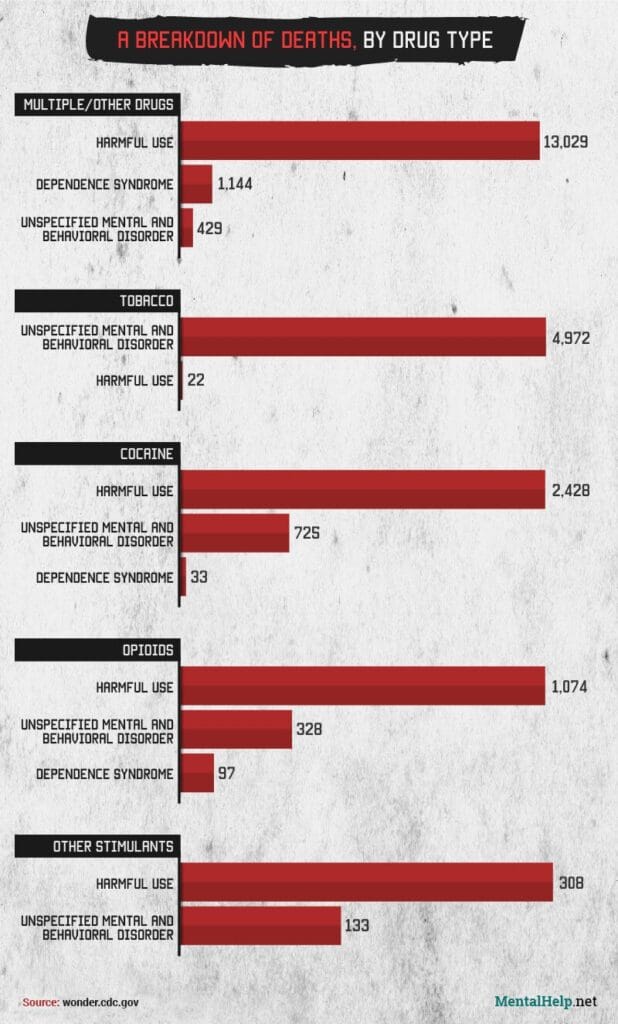
The risk to mental health is even clearer when looking at the number of deaths attributed to mental conditions related to the use of a drug versus deaths due to the drug itself. Among deaths linked to cocaine between 1999 and 2013, mental health conditions accounted for 22.8%, compared with 76.2% attributed directly to use of cocaine.
Similarly, 21.9% of deaths linked to opioid use were caused by mental disorders. And for deaths due to stimulants other than cocaine, 30.2% were associated with drug-related mental conditions rather than stimulant use itself. These data show that for drug users, the potential consequences to their physical health aren’t the only issue to worry about – mental health disorders can be just as deadly.
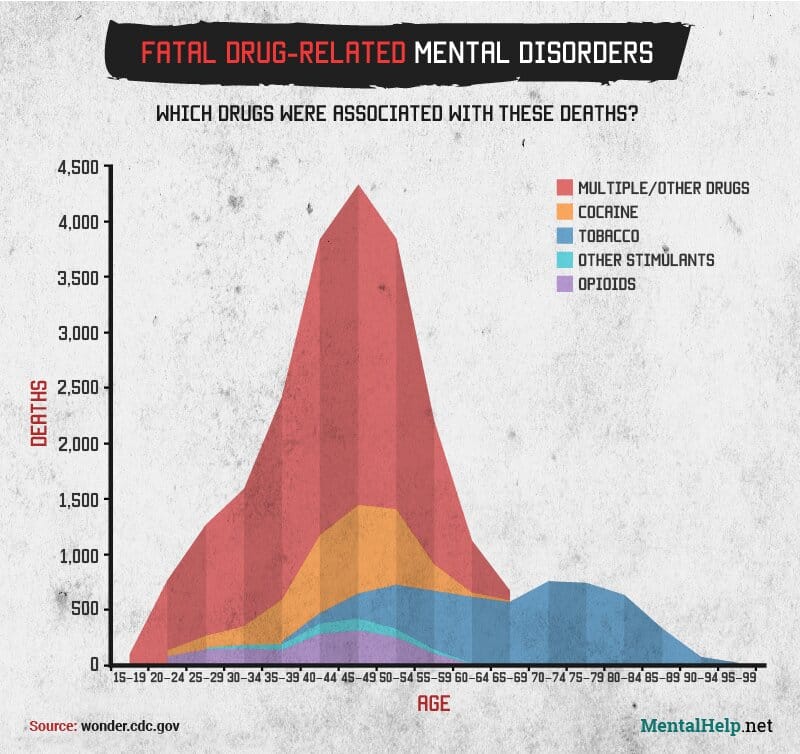
We also looked at the impact of deaths from drug-related mental conditions by age group, examining the effects of different substances across a lifetime. Of all the specifically named drugs, cocaine-related mental disorders showed the highest peak, at nearly 1,500 deaths among those aged 45 to 49. The categories of other stimulants and opioids each peaked in the 45 to 49 age group as well, but with fewer than 500 deaths at peak. For all of these specific substances, the number of deaths attributed to drug-related mental disorders began to climb sharply after age 34.
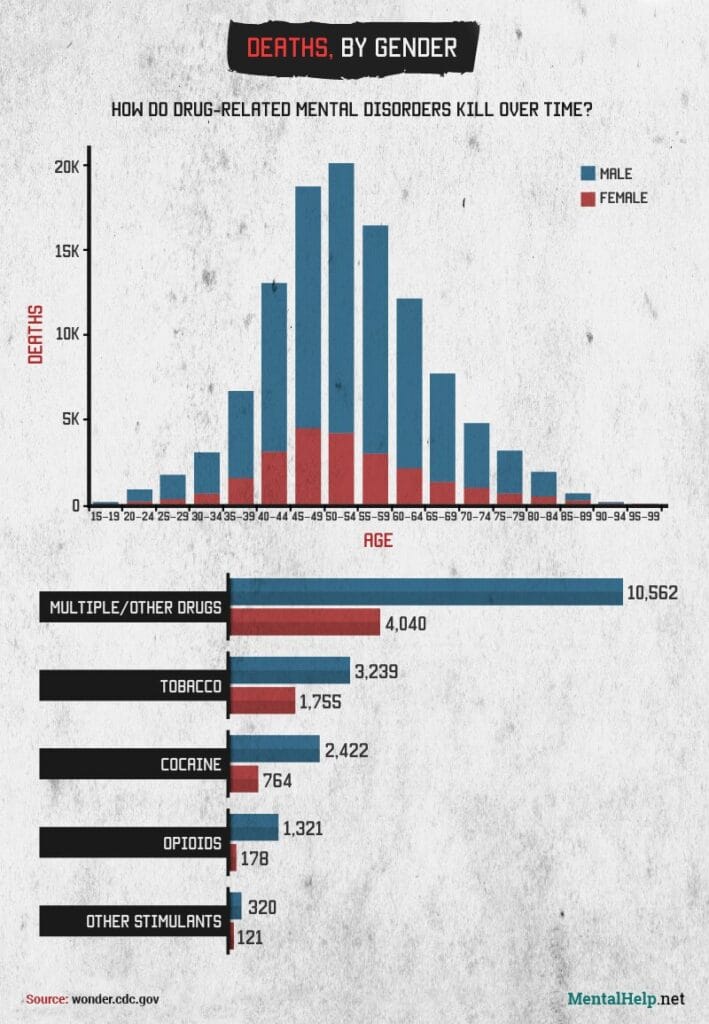
Finally, we examined the total number of drug-related mental disorders by gender. For all substances, deaths among men were substantially more frequent than deaths among women. Given that substance abuse is more common among men and mental health conditions are more common among women, this shows the substantial role that drugs can play in the development of potentially deadly psychiatric disorders. Notably, deaths due to drug-related mental conditions peak at an earlier age for women – ages 45 to 49, compared with 50 to 54 among men.
Seeking Help for Substance Use and Mental Health Conditions
Coping with mental illness is a struggle that millions of people face every year. But while turning to drugs or alcohol may seem to provide temporary relief, substance use can ultimately make the challenges of mental health conditions even greater. Co-occurring substance use and psychiatric disorders can be complex and unique for every individual, and you deserve expert help tailored to meet your personal needs.
Methodology
Data on the 2014 prevalence of mental illness and drug use, abuse and dependence among the population was taken from the U.S. Substance Abuse and Mental Health Services Administration’s 2014 National Survey on Drug Use and Health. Mortality data were obtained from the U.S. Centers for Disease Control and Prevention’s WONDER Multiple Cause of Death database, spanning the years 1999 through 2013 and searching within detailed mortality for ICD-10 codes F10 through F19 (mental and behavioral disorders due to psychoactive substance use). No results were found for cannabinoids, sedatives or hypnotics, hallucinogens, or volatile solvents. Due to the large number of deaths attributed to alcohol-related mental disorders compared to other substance-related mental disorders, alcohol was excluded from further analysis after the first section to avoid substantially skewing the data.
- http://wonder.cdc.gov/
- http://www.samhsa.gov/data/sites/default/files/NSDUH-MHDetTabs2014/NSDUH-MHDetTabs2014.htm
- http://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs2014/NSDUH-DetTabs2014.pdf
- http://www.apa.org/helpcenter/alcohol-disorders.aspx
- http://www.healthinfonet.ecu.edu.au/uploads/workers-portal/polydrug-use.pdf
- http://www.ncbi.nlm.nih.gov/pubmed/20863629
- http://www.samhsa.gov/data/sites/default/files/NSDUHmhfr2013/NSDUHmhfr2013.pdf
We are a health technology company that guides people toward self-understanding and connection. The platform provides reliable resources, accessible services, and nurturing communities. Its purpose is to educate, support, and empower people in their pursuit of well-being.
We take mental health content seriously and follow industry-leading guidelines to ensure our users access the highest quality information. All editorial decisions for published content are made by the MentalHealth.com Editorial Team, with guidance from our Clinical Affairs Team.
Further Reading
We are a health technology company that guides people toward self-understanding and connection. The platform provides reliable resources, accessible services, and nurturing communities. Its purpose is to educate, support, and empower people in their pursuit of well-being.