Physical Versus Mental Illness

One in four people in the world will experience a mental or neurological illness at some point in their lives.
Nearly two-thirds of those with a known mental illness never seek professional treatment.
Common misperceptions and stigma surrounding mental health conditions may deter people from seeking treatment, but just how pervasive are these judgements?
To understand the influence of stigma surrounding mental illness, we polled over 2,000 people to find out how they respond to issues of mental health and physical health. The results indicate that Americans still have far to come in reducing the shame associated with mental illness.
ADMITTING TO HAVING A MENTAL ILLNESS

Major depressive disorder affects more than 15 million adults in the U.S. and is currently the leading cause of disability for people aged 15 to 44. While depression may be confused with sadness or anti-social behavior, major depressive disorder is defined as a form of depression that does not correct itself naturally and can present serious symptoms like anxiety, fatigue, lack of interest in hobbies or activities, and even thoughts of death or suicide.
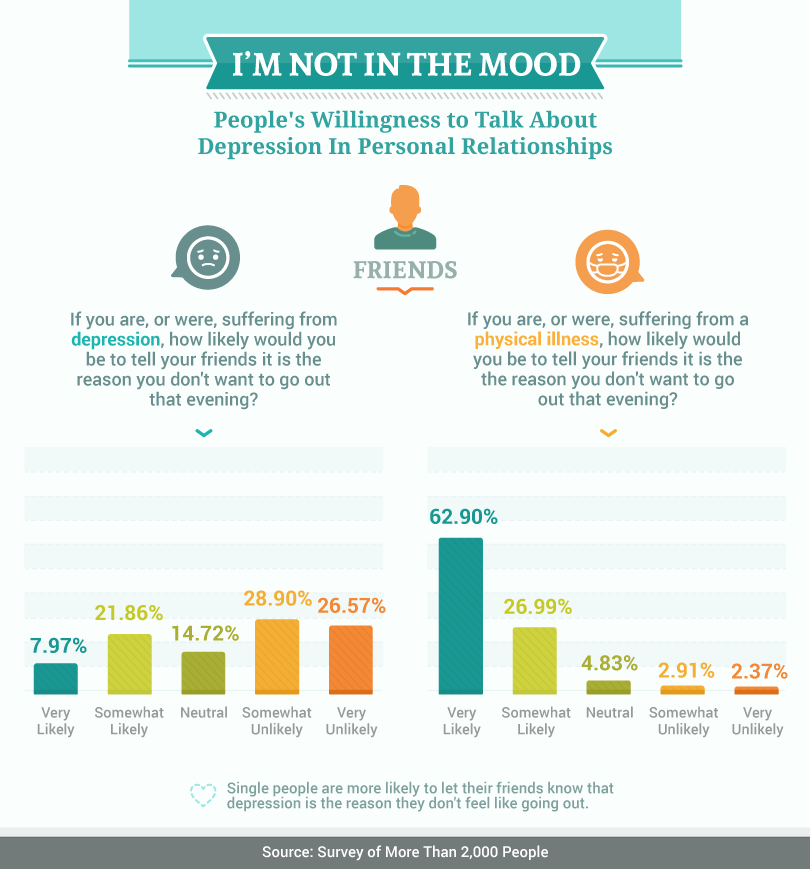
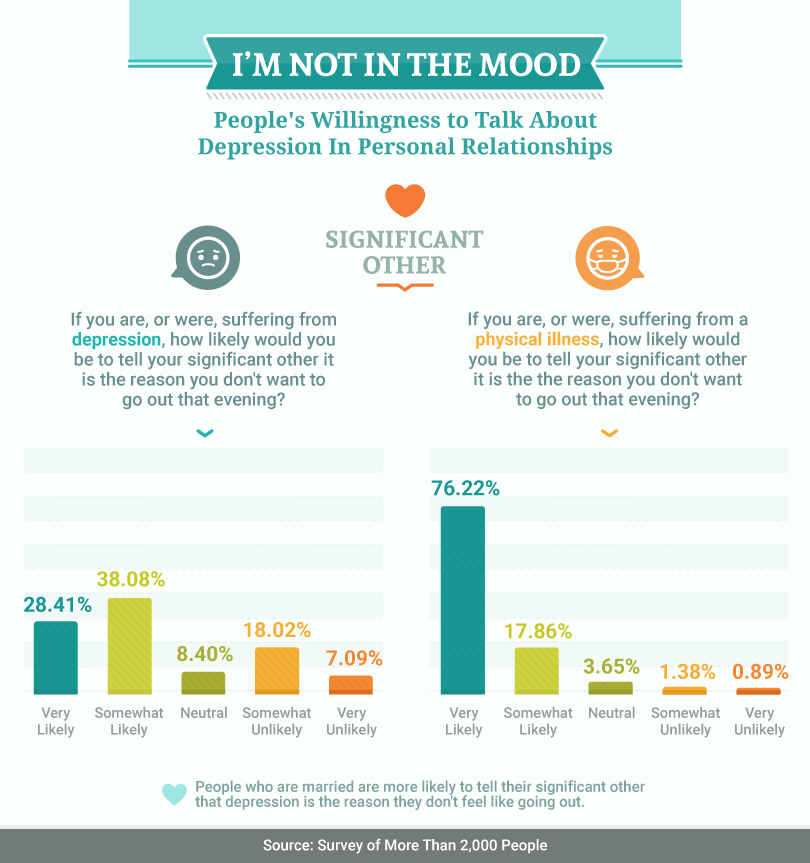
Considering the effects of this condition, we asked respondents how likely they would be to admit they weren’t interested in going out or engaging in social activity due to feelings of depression. Less than half of our survey respondents said they would disclose their mental health status to a family member or friend in this scenario – about 30 percent noted they were “somewhat likely” or “very likely” to share their mental health concerns with friends, while about 41% said they were at least “somewhat likely” to share with family. Respondents were more likely to share their mental illness with significant others, with about 66 percent agreeing that they were at least “somewhat likely” to tell their significant other that they felt unenthusiastic about socializing due to depression.
In comparison, the vast majority respondents were “somewhat likely” or “very likely” to admit to their family, (about 90 percent), friends, (about 89 percent), and significant other (about 94 percent) that a physical illness was preventing them from going out or engaging in social activity.
It’s evident that the survey respondents did not believe their mental health would be accepted as a legitimate health concern equivalent to a physical ailment. Our survey reveals a clear delineation between how Americans think about mental health and physical health. Without more open conversations surrounding mental health, those who are suffering may stall progress in seeking help and support.
MENTAL ILLNESS IN THE WORKPLACE

When we asked respondents how likely they would be to tell their boss that a mental illness was the reason they couldn’t come into work, participants overwhelmingly said they were very unlikely to be honest about their mental health (about 59 percent). In contrast, the majority of our participants were very likely to share their physical ailment with their boss (almost 63 percent).
Many people perceive depression as a personal form of weakness, rather than a serious illness that comes from biochemical, environmental, and genetic factors. As such, people may be afraid to admit when they experience symptoms. At work, those suffering from depression may even be afraid of losing their job.
Depression in the workplace is a serious concern. Depression accounts for over 217 million lost work days every year and studies show that workplace suicides are on the rise. Data from 2003 to 2010 indicates that more than 17,000 workers took their own lives – averaging 1.5 suicides for every one million workers. These suicide rates were 15 times higher for men than for women, and four times higher for workers between 65 and 74 years old.
Some companies have made efforts to increase education around mental health among employees to help reduce the stigma surrounding mental illness and to encourage understanding and support among coworkers. Corporations that have adopted mental wellness programs have opened up pathways between employees and upper management for open dialogue about mental health concerns.
DELAYED TREATMENT
Despite the serious nature of depression and other mental illnesses, research suggests that many adults who suffer from these conditions don’t just delay treatment – they avoid it completely.
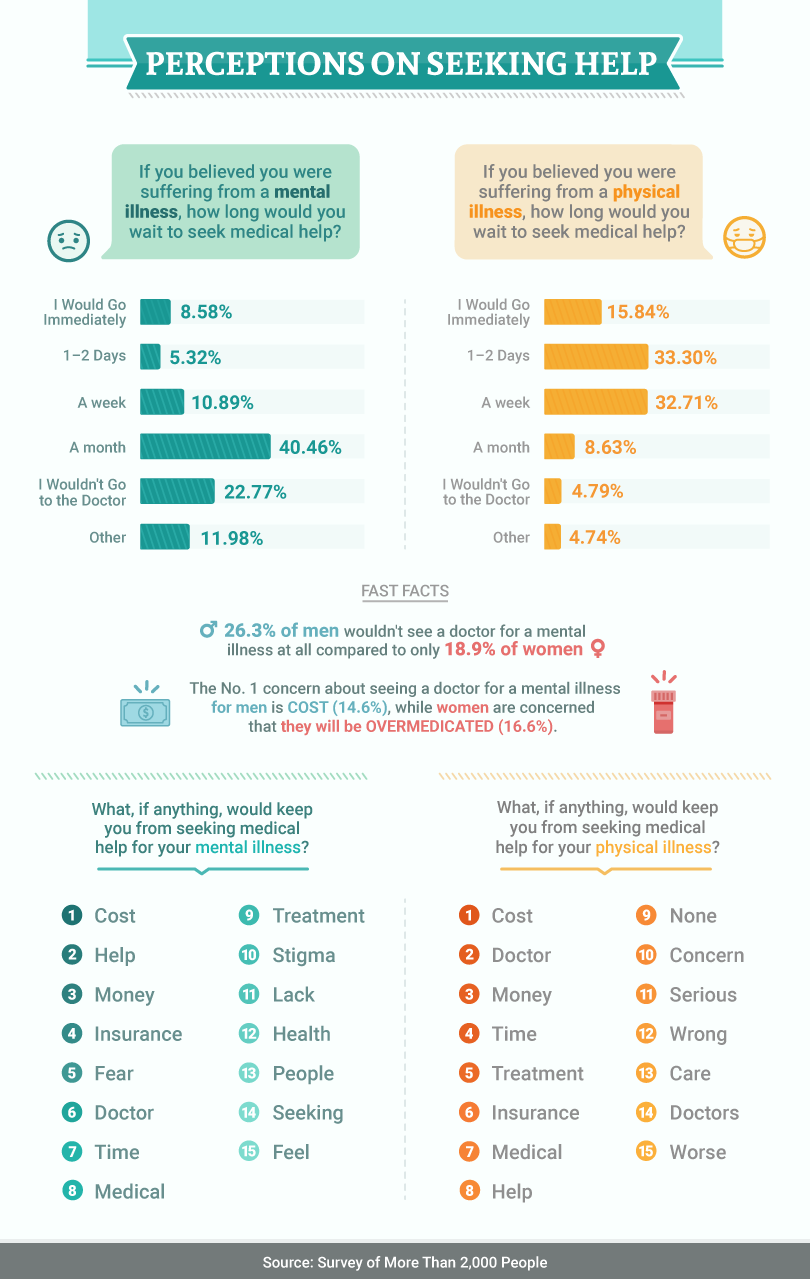
When we asked our participants how long they would wait to seek medical help if they were suffering from a mental illness, over 40 percent admitted they would wait a month to pursue treatment, while almost 23 percent said they wouldn’t seek help at all. Comparatively, 66 percent of respondents would not wait longer than one week to seek treatment for a physical ailment.
The delay of seeking medical attention for a mental illness can be tragic. The long-term effects of untreated depression can include cardiovascular disease, substance abuse, and higher rates of mortality. Long term depression has also been linked to increased risk of heart attacks brought on by a combination of the symptoms of depression and stress within those who have heart disease. Depression is the psychiatric diagnosis most commonly associated to suicide.
So why do most people avoid treatment for mental illness? The most common barriers include stigma, fear, embarrassment and finances. The history of mental health stigma in the U.S. is long and varied, but studies have shown that education and personal contact with someone who suffers from conditions like depression can have a positive impact on the perception not just of their condition, but hope in their chances of recovery. Sadly, many suffering from depression do not realize the full severity of their conditions or the effects of delaying treatment. One respondent in our survey, said that the “concern over discrimination and concern over the effect of a positive diagnosis on [his or her] self esteem,” was what prevented him or her from seeking help for a potential mental illness.
DESCRIBING THE STIGMA

To better understand how respondents perceived stigma surrounding mental illness, we asked them why they felt uncomfortable discussing their mental health. The responses revealed some disheartening patterns – words such as “weak” “judgement” “stigma” and “not understanding” were common.
Despite research linking mental illness to biological and genetic factors, there are still misperceptions surrounding those who suffer from depression. Stigma continues to play a role in discouraging individuals from seeking treatment for mental illness.
We also asked respondents to write down their concerns about seeking help for a mental illness. Terms such as “problem,” “medicine,” “drugs,” and “side effects” were frequent, indicating a concern and possible misunderstandings surrounding the methods used to treat mental illness. While prescription medication is often used for treating severe depression, cognitive behavioral therapy (CBT) has been found to effectively treat depression as well. CBT is a form of “talk therapy” which aims to help a patient recognize distorted thinking to change his or her patterns of thought.
THE GREAT DIVIDE
Our survey indicates that Americans do not view mental health conditions as a threat equivalent to a physical ailment. When it comes to talking about mental health with friends, family, or coworkers, respondents simply aren’t comfortable being honest. As a result, too many Americans avoid treatment for common mental health conditions.
METHODOLOGY
We surveyed over 2,000 people in the United States about their willingness to discuss depression and physical illnesses to uncover what people are comfortable talking about, or not.
- http://www.who.int/whr/2001/media_centre/press_release/en/
- https://www.adaa.org/about-adaa/press-room/facts-statistics
- https://www.nimh.nih.gov/health/topics/depression/index.shtml
- http://www.depressioncenter.org/work/depression-and-work/stigma/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3077049
- https://www.scientificamerican.com/article/most-depressed-adults-in-the-u-s-remain-untreated
- http://www.livestrong.com/article/69705-longterm-effects-untreated-depression/
- http://www.suicidology.org/Portals/14/docs/Resources/FactSheets/2011/DepressionSuicide2014.pdf?ver=2014-09-05-173218-107
- http://depressiongenetics.stanford.edu/mddandgenes.html
- http://www.nature.com/mp/journal/v21/n6/pdf/mp201569a.pdf
- http://www.who.int/mediacentre/factsheets/fs369/en/
- https://www.psychiatry.org/patients-families/depression/what-is-depression
- http://www.huffingtonpost.com/2014/11/13/mental-illness-physical-i_n_6145156.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC486942
- https://www.ncbi.nlm.nih.gov/pubmed/22854096
- http://www.usnews.com/articles/2015/03/13/mental-health-a-new-priority-in-corporate-america
- http://www.huffingtonpost.com/joseph-rauch/employers-talk-about-mental-illness-workplace_b_11427674.html
- http://www.npr.org/sections/health-shots/2016/07/02/484055668/community-based-care-can-reduce-the-stigma-of-mental-illness
- http://www.theatlantic.com/health/archive/2013/08/why-i-keep-my-bipolar-disorder-secret-at-work/278931/
We are a health technology company that guides people toward self-understanding and connection. The platform provides reliable resources, accessible services, and nurturing communities. Its purpose is to educate, support, and empower people in their pursuit of well-being.
We take mental health content seriously and follow industry-leading guidelines to ensure our users access the highest quality information. All editorial decisions for published content are made by the MentalHealth.com Editorial Team, with guidance from our Clinical Affairs Team.
Further Reading
We are a health technology company that guides people toward self-understanding and connection. The platform provides reliable resources, accessible services, and nurturing communities. Its purpose is to educate, support, and empower people in their pursuit of well-being.